Health and Wellness: Should You Get the Shingles the Vaccine?
- Tuesday, 20 August 2019 14:31
- Last Updated: Tuesday, 20 August 2019 14:35
- Published: Tuesday, 20 August 2019 14:31
- Stacie M. Waldman
- Hits: 7402
 Anyone who has lived through an episode of shingles has a story and the stories are all similar. Victims of the nasty virus bemoan the extended length of the illness (a few weeks to a couple of months), the extreme and unrelenting pain experienced and the shock of the diagnosis. Should you get the vaccine and spare yourself the pain?
Anyone who has lived through an episode of shingles has a story and the stories are all similar. Victims of the nasty virus bemoan the extended length of the illness (a few weeks to a couple of months), the extreme and unrelenting pain experienced and the shock of the diagnosis. Should you get the vaccine and spare yourself the pain?
“The worst pain of my life was from shingles. The second worst was after having three C-sections.” This is how one young mom described her experience with shingles. Her case never progressed to blisters because she quickly began taking an anti-viral medication thanks to a rapid diagnosis, but she still experienced the excruciating burning pain that people often associate with shingles. She was in her mid-30s.
Andy, a corporate lawyer who lives in the Heathcote area, was initially diagnosed with an eye and sinus infection and given a course of antibiotics. A couple of nights later, the pain in his face got so bad that his wife had to call a doctor at midnight and beg for pain medication. He mentioned to the on-call doctor that he had a strange blister on his nose as well; that doctor immediately and correctly diagnosed Andy with shingles. The pain, swelling and blistering got worse as he began anti-virals, then slowly got better over a month. An infection persisted in his eye, however, and he could barely see at one point. He was scared he would lose his eyesight. It was almost impossible to work. As the eye infection began to clear with the help of a corneal specialist, the itching phase started. “Mentally, this proved to be the most devastating part of the whole experience,” Andy said. “The itching was out of control, I could not stop it, it affected every aspect of my existence. I walked around at home and at work with ice packs on my head to try to numb things…when the itching flared up, I did what I could to exist but really I couldn't do anything else,” he added. Although Andy has mostly recovered, he does still have episodes of intense itching in his scalp and around his eye. Andy was in his late 40s at the time.
Joyce had her daughter in July of 2015, moved to Scarsdale in August, went back to work in October and hosted eight additional people for Thanksgiving. “I think it was stress that activated the shingles,” she said. “I had to fly to a conference the Monday after Thanksgiving… and I went with a rash on my forehead thinking it was contact dermatitis. When I got back from my conference,” she continued, “I remember being in a lot of pain…I went to [an urgent care] and the … doctor there took one look at me and said it was shingles.” She was put on anti-virals and saw an eye doctor to make sure she had no eye complications. “It cleared up after 4-5 weeks, but I have some scarring on my forehead from the blisters.” Joyce was 35 at the time.
Sarah’s shingles began with a tingling sensation under her rib cage, deep under the skin. She felt like she had been punched but couldn’t see any signs of injury. The pain got worse and she developed small bumps that resembled bug bites at first, but quickly grew into a very painful rash. She saw diagnosed around day 4 and was given anti-virals but doesn’t think it helped much. It took 6-8 weeks for the pain to go away. “At times, I could barely move off the couch and it was very difficult to sleep,” she said. “I could barely wear a bra. I had a bad scar on my mid-section that took a very long time to heal.” She approached her doctor about getting the vaccine after her shingles subsided but was told there was a vaccine shortage and couldn’t get it, even if paying cash and even though she is a Type II diabetic (and higher risk) until she is 50. “…every little twitch I feel in my body makes me paranoid that I have shingles again. I went to the doctor last week insisting I be seen urgently because I thought I had shingles again, but it turned out to be just a series of bug bites,” she said. “I felt a little silly but I just couldn’t imagine going through the disease process again.” Sarah was 37 when she had shingles.
Many others shared stories like this and all emphasized the importance of being diagnosed properly and in a timely manner. According to CDC (Centers for Disease Control and Prevention), the incidence of shingles is increasing. Research is ongoing to determine why this upward trend is continuing.
How is shingles diagnosed and what is it like?
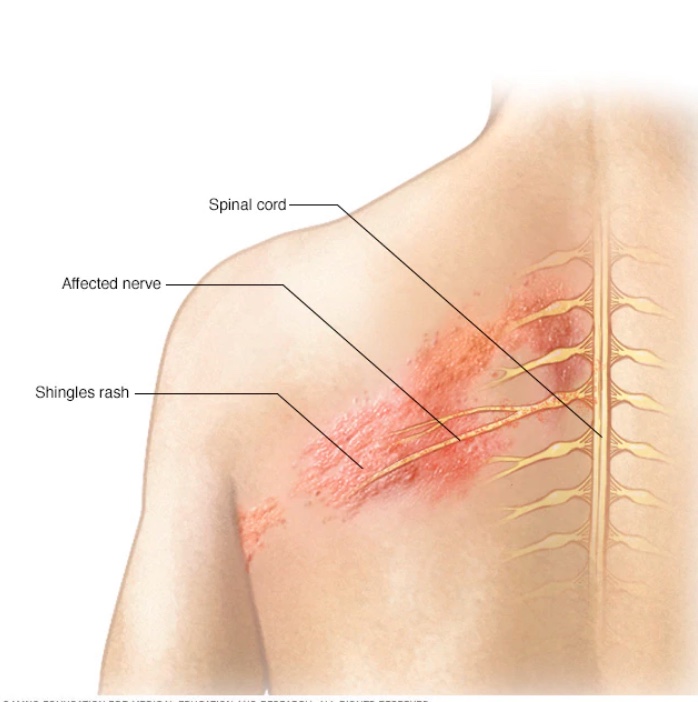
Shingles can present in a multitude of ways. It often presents as a painful “burning” rash on one side of the face or body, most commonly the mid-section. Some people never develop a rash and some people develop a rash but have little pain associated with it, others develop blisters that are extremely painful; some blisters are not painful at all. The blisters scab over in a week to 10 days. “The …thing I didn't know, but I do now, is that having pain on just one side of the face [or body] is…a telltale sign of shingles,” said Andy. Other common symptoms are fever, headache, chills and upset stomach. Most people recover fully within 2-4 weeks. Diagnosis can be tricky as shingles can mimic other infections and it does not present the same way in every patient. “The other thing I learned from my experience,” added Andy, “is that every day that passes can significantly increase the severity of the infection.” Joyce, like many people, incorrectly thought that shingles mainly affects older people. Several people who responded to me said that their shingles was so bad and lasted so long that they felt depressed during the illness.
Can shingles be treated?
An anti-viral drug can be used after diagnosis to reduce the length and the severity of the illness. Correct diagnosis of shingles early on is important for the treatment to work. For Andy, the delay in his diagnosis (about two weeks) likely increased the severity of his case of shingles. For the young mom of 3, early diagnosis and treatment likely prevented her from having a more severe case of shingles. Treatment for the itching includes typical anti-itch creams and medications. Oatmeal baths can help soothe the skin as well.
Are there any long-term effects from shingles?
Long term effects from shingles can occur. Post-Herpetic Neuralgia (PHN) is severe pain at the sites of the shingles rashes that last for months or even years. It occurs in 10-18% of people and the pain from it can be completely debilitating.
Other potential long-term problems include vision loss if shingles occurs near the eye, nerve damage causing facial paralysis or hearing and balance problems, and skin infections as a result of the blisters and itching. Although Andy’s eyesight has completely returned, he has small scars inside his eye that occasionally make his vision a bit cloudy. “I continue to get some itching in my scalp and more frequently around my eye, but these are just momentary events that don't impact my life in any way,” he said. Andy also has some dead spots (no feeling) on his nose from the more severe blisters.
Is shingles contagious?
Shingles is caused by the reactivation of the virus that causes chickenpox. It can affect anyone who has had chickenpox or has not been vaccinated against it. After a person has had the chickenpox, the virus lies inactive in nerve tissues near your spinal cord and brain. If the immune system is weakened, the virus may start to multiply along the affected nerve pathway eventually reaching the skin. Therefore, although shingles itself is not contagious, a person with shingles can infect someone with the chickenpox virus (during the blister phase) if they have not been previously exposed or vaccinated. It is recommended that people with shingles remain isolated from babies, the elderly and people who are immunocompromised. Andy said that people would often ask him if his shingles was contagious. “I would have to explain to them that you can't catch shingles from another person, it's always a reactivation of virus already in your body. Many people don’t understand how a person gets shingles.”
Can shingles be prevented?
A shingles vaccine (called Shingrix) is available and recommended by CDC (Centers for Disease Control and Prevention) for healthy adults ages 50 and up. The vaccine is administered in two doses, 2-6 months apart. It is more than 90% effective at preventing shingles and provides protection longer than the previous approved vaccine called Zostavax. Your doctor’s office should carry the vaccine and most pharmacies will provide it as well. A person can get shingles more than once. It is important to note that people under 50 can and do get shingles, but the risk of serious side effects from shingles is less.
Does the vaccine have side effects?
Most side effects are limited to redness and soreness at the injection site like any other vaccine. Some people felt tired, had muscle pain, a headache, shivering, fever, stomach pain, or nausea. In fact, Andy had fever, chills and nausea from the vaccine, but it cleared up overnight. About 1 out of 6 people who got Shingrix experienced side effects that prevented them from doing regular activities. Lisa from Heathcote had a small reaction to the booster from Shingrix (low fever and sore arm) but she argues that it’s completely worth getting the vaccine. “My husband had no side effects,” she said. “My mom got the original vaccine but unfortunately got shingles while she was undergoing radiation treatment for cancer right before she had planned to get the updated vaccine. She ended up in the hospital on IV drips of morphine and anti-virals…she was in a lot of pain.”
The response I got on the Scarsdale Moms Facebook from a post asking for people to share their experiences with shingles and/or the vaccine was overwhelming and thank you to all who replied. I couldn’t share all of your stories, but please feel free to share in the comments. Shingles can be severe and it is does not only affect the elderly. In fact, of the 15 responses I received from people who got shingles, only one person was over the age of 50. The vaccine cannot cause shingles. Shingles itself is not contagious but can cause chicken pox in an unvaccinated person or in someone who never had chicken pox. Everyone who responded with a shingles experience stressed how important it is to recognize (or have a doctor recognize) the signs and symptoms early so treatment can begin before the pain or disease severity increases. Talk to your doctor to learn more about vaccination.