150 Scarsdale Residents Learn CPR
- Details
- Category: Health
 According to the National Heart, Lung, and Blood Institute, cardiac arrest results in about 300,000 to 450,000 deaths in the United States each year. Cardiac arrest is a medical emergency that requires immediate medical attention—90% of people who have a cardiac arrest outside of a hospital die within minutes due to insufficient blood flow to vital organs. However, the American Heart Association states that the immediate administration of cardiopulmonary resuscitation (CPR) to a patient can double or even triple that person’s chance of survival.
According to the National Heart, Lung, and Blood Institute, cardiac arrest results in about 300,000 to 450,000 deaths in the United States each year. Cardiac arrest is a medical emergency that requires immediate medical attention—90% of people who have a cardiac arrest outside of a hospital die within minutes due to insufficient blood flow to vital organs. However, the American Heart Association states that the immediate administration of cardiopulmonary resuscitation (CPR) to a patient can double or even triple that person’s chance of survival.
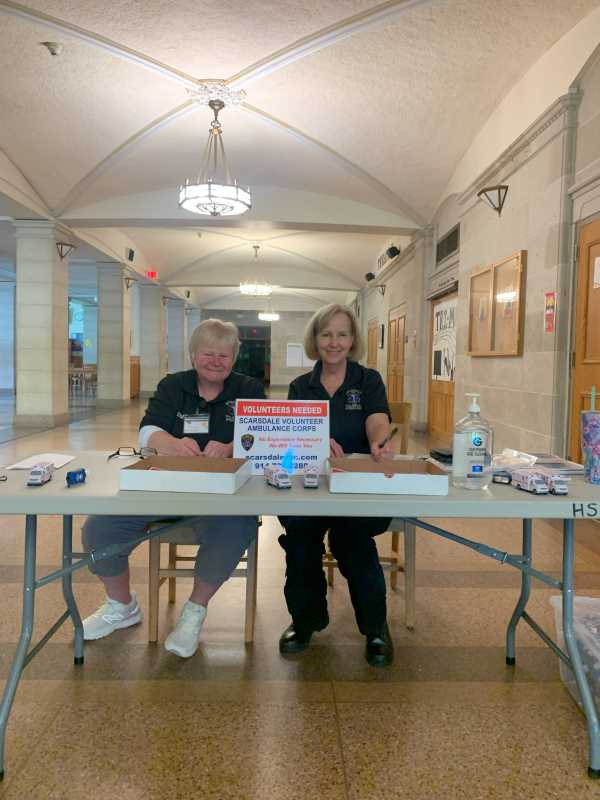
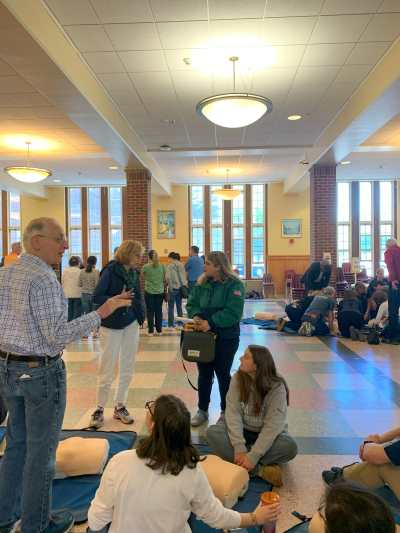
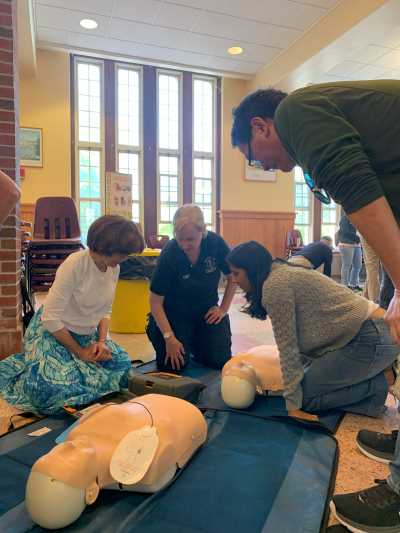
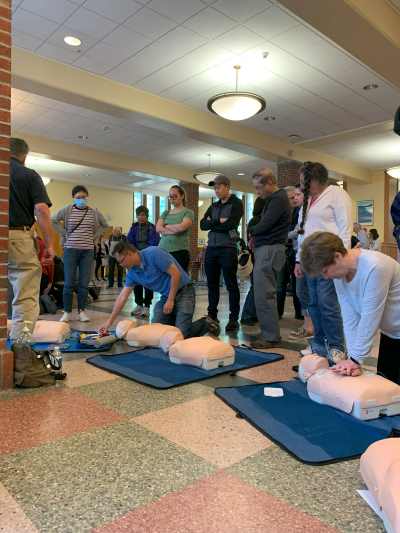
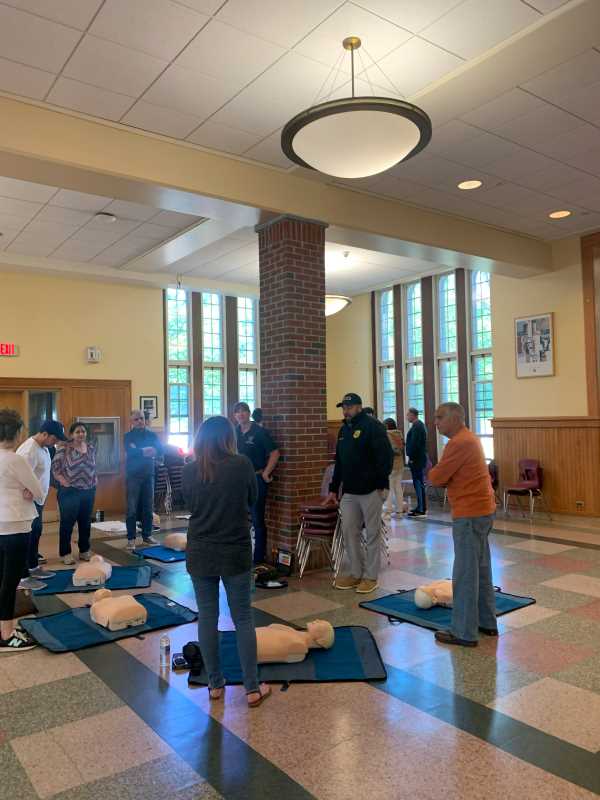
Recognizing that bystander intervention is a critical aspect of pre-hospital care, Scarsdale Volunteer Ambulance Corps (SVAC) organized a Friends & Family CPR Class at the Scarsdale Public Highschool. Morning and afternoon training sessions were hosted on May 7th, 2023, where a total of 150 residents learned how to perform hands-only CPR. The program was truly a community effort, with instructors from SVAC, Larchmont Volunteer Ambulance Corps, and Irvington Volunteer Ambulance Crops attending to teach. The combined effort of the participating organizations was essential to the success of the program.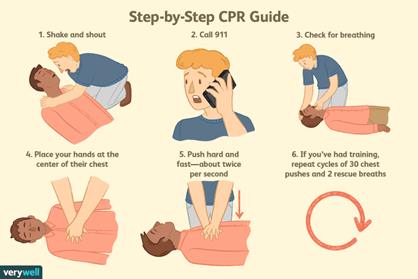
According to Angela Manson, a dedicated member of SVAC, the organization is always looking for new volunteers. Manson stated that SVAC runs year-round EMT classes and that no experience is needed to participate in their programs. Above all, she emphasized that the programs would equip participants with the knowledge and skills needed to manage medical emergencies. More information on available courses can be found here.
Steamed Mussels: A Heart-Healthy Recipe from Half Moon Restaurant
- Details
- Written by: Joanne Wallenstein
- Category: Health
 As part of the “What the Doctor Ordered” series from White Plains Hospital, they asked some local restaurants to create heart-healthy meals with five cardiologist-approved ingredients. White Plains Hospital Director of Cardiogenetics Dr. Marc Waase challenged Andy Bennett, Executive Chef at Half Moon Restaurant, to create a dish using mussels, almonds, chickpeas, oranges, and low-fat Greek yogurt.
As part of the “What the Doctor Ordered” series from White Plains Hospital, they asked some local restaurants to create heart-healthy meals with five cardiologist-approved ingredients. White Plains Hospital Director of Cardiogenetics Dr. Marc Waase challenged Andy Bennett, Executive Chef at Half Moon Restaurant, to create a dish using mussels, almonds, chickpeas, oranges, and low-fat Greek yogurt.
Chef Andy created a Steamed Mussels dish with Spinach and Almond Pesto, paired with Chickpeas and Oranges.
Heart-Healthy Benefits Include:
• Oranges are a great source of fiber and potassium.
• Mussels are high in omega-3 fatty acids.
• Almonds help keep blood vessels healthy, reducing heart disease risk.
• Greek yogurt offers twice the protein of traditional yogurt.
• Chickpeas are high in magnesium and potassium.
Try this delicious meal at Half Moon or using the recipe below.
Steamed Mussels with Spinach & Almond Pesto, Chickpeas and Oranges
Makes 2 entrees or 4 appetizers
Sauce
4 oz. Spinach – washed
2 Tbsp. Chopped parsley
2 Cloves garlic – chopped
0.75 oz. Toasted Almonds – chopped
3.5 oz. Olive oil
1 Orange – zested, (segments and juice reserved)
1/8 tsp. Chili Flakes
1/8 tsp. Za’atar spice blend
1.75 oz. Plain Greek yogurt
Salt to taste
Dish
2 lbs. Mussels – cleaned
4 oz. Canned Chickpeas
4 Tbsp. Water
1 Orange – segments and juice from above
Instructions
1. Place all the sauce ingredients except the yogurt into a food processor.
2. Blend until everything is combined.
3. Add the yogurt and mix enough to combine. Check seasoning.
4. Preheat a large pot or sauté pan.
5. Add mussels, chickpeas and 4 Tbsp. of water.
6. Cover with a lid until the all mussels have opened.
7. Remove the lid and add in the sauce so it combines with all the cooking liquid.
8. Pour everything into a large serving bowl and sprinkle the orange segments on top.
Notes:
• It’s great to serve alongside some thick-sliced crusty bread for mopping up the broth.
• Be careful when seasoning — there is a natural amount of brininess from the mussels already. Season lightly and you can add more at the end if needed.
Half Moon is located at 1 High Street in Dobbs Ferry, NY. For reservations, visit halfmoonhudson.com or call (914) 693-4130.
A Clinical Trial Led to One Woman’s Triumph Over Lung Cancer
- Details
- Written by: Joanne Wallenstein
- Category: Health
 (This article was submitted by White Plains Hospital)
(This article was submitted by White Plains Hospital)
Renee Davis was terrified to learn she had lung cancer. But White Plains Hospital’s excellent doctors — and its access to a cutting-edge clinical study — gave her hope for a cure.
It’s hard to imagine how a health emergency could turn out to be a positive. But that’s exactly what it was for Renee Davis, 67, a White Plains resident and supermarket clerk. Although her crisis was a severe allergic reaction, it uncovered another potentially deadly problem: lung cancer.
Davis’ journey began in late 2019, when, out of the blue, she felt an odd sensation on her face. “I looked at it in the mirror and thought, Holy smokes!” she recalls. “It was all swollen.” Soon, she began to have trouble breathing. She drove to urgent care and was sent immediately to White Plains Hospital’s Emergency Department, where she was admitted to the Intensive Care Unit. The physicians worked to stop the swelling and keep her airway open. Fortunately, after two days, she recovered. The likely allergen was identified as Davis’ blood pressure medication, and she was switched to a different drug.
Yet her worries weren’t over: the CT scan she received during treatment showed an unexplained mass. At a follow-up visit, she was directed to see Dr. Todd Weiser, the Hospital’s Director of Thoracic Surgery. Davis was understandably ner¬vous, wondering what would come next, but as soon as she met Dr. Weiser, she felt she could trust him.
“He was so nice and didn’t speak to me like he was superior to me,” she says. He quickly arranged for Davis to have a PET-CT scan, which would provide more detailed information on the changes in her lungs.
What he saw was concerning. “The scan showed a large mass that was in the central part of her right lung, and the lymph nodes within her lung were enlarged,” Dr. Weiser says. He performed a lung biopsy as soon as possible, and it showed she had stage 2 lung cancer.
Davis was devastated by the news, but Dr. Weiser reas¬sured her. “He told me he had my back and was going to do surgery to remove it,” she says. “Still, I went into the bathroom and fell to my knees. I wondered what I was going to tell my family. My older son was getting married in Mexico in July. I didn’t know if I’d be able to go to the wedding.”
Entering a Clinical Trial
The more immediate concern was to figure out what, in addition to surgery, would give Davis the best chance of a complete recovery. At Dr. Weiser’s recommendation, Davis met with Dr. Dan Costin, Director of the White Plains Hospital Center for Cancer Care, who proposed that she enter a clinical study on lung cancer treatment in which the Hospital was participating.
“It’s called Keynote 671,” Dr. Costin says. Participants, he explains, are divided into two groups. Both undergo chemotherapy before surgery rather than afterward, which is the standard treatment plan. In addition, during chemotherapy, half the patients receive immunotherapy, a treatment that helps the body’s immune system fight cancer. The other subjects receive a placebo.
The purpose of the study is to establish immunotherapy’s usefulness for treating lung cancer at earlier stages of diagno¬sis. “We know it works very well if you have very advanced or stage 4 lung cancer,” Dr. Costin says. “Renee’s cancer was at an early stage, but it’s a stage where, unfortunately, a significant number of patients are destined to have a recurrence, even when they’ve had surgery and standard chemotherapy.”
The trial, he told Davis, could potentially allow her to receive pem¬brolizumab, an immunotherapy drug that makes it difficult for cancer cells to hide from the immune system.
Despite knowing that the research project might give her access to cutting-edge treatment, Davis was hesitant. Her husband and two sons also had reservations, wondering if the experimental drug might have unforeseen health consequences.
“But then Dr. Costin explained it all to us during a visit,” Davis says. “He showed us photographs of different stages of cancer and explained why I was a very good candidate for the study and could potentially be helped a lot.” She and her family were convinced. “My older son said, ‘Mom, what do you have to lose?’”
The details of the study and treatment were further explained to Davis by Catherine Reilly, MPH, RN, a Clinical Research Nurse with the White Plains Hospital Center for Cancer Care. “I take care of patients who are enrolled in clinical trials,” Reilly explains. “In my initial discussions with them, we talk about the research study as a possible treat¬ment option. I tell them about the purpose of the study and give them all the details. I also ensure that the patients meet the eligibility requirements for the clinical trial.
“In addition, at any given time, we have approximate¬ly 30 trials that are actively enrolling patients and other studies with patients in follow-up,” Reilly continues. The Hospital is playing a key role in the pembrolizumab study, she notes, as one of 42 other research sites worldwide. The fact that White Plains Hospital was selected to be part of this curated handful reflects its excellence, she adds.
“We have built a state-of-the-art, cutting-edge Cancer Center, and as part of it, we have invested in developing a strong clinical trials office with an outstanding director and an excellent supporting staff,” says Dr. Costin. “We have also been able to convey the importance of clinical trial partic¬ipation to physicians and providers caring for our cancer patients. And we have an established oncology pharmacy with an interest and expertise in clinical research. As a result, our program has been very attractive when sites are being selected for clinical trials.”
Facing the Challenge Bravely
Davis began what would be the first of four IV treatments in January 2020. “The people at the infusion center were really nice. They treated me with such kindness,” she shares. But that wasn’t the only good news: Davis also felt no adverse effects from the chemotherapy and (possible) immunotherapy. She went into each infusion session with an upbeat attitude, even wearing fancy outfits a couple of times. “The nurses asked me where I was going, and I told them I just came here like that because I hadn’t worn those kinds of clothes in a while, so I thought I’d get dressed up,” she says.
All wasn’t cheerful, however. In March, just as Davis was preparing for her third infusion, the pandemic began. “Suddenly, we were in a situation where we were wondering if we could even bring our patients in to get standard chemo¬therapy, let alone if they were in clinical studies,” Dr. Costin says. However, White Plains Hospital took every possible step to make sure non-COVID patients were kept safe, and Davis still got the attention she needed. “We placed her on high priority. She never missed a treatment,” Dr. Costin explains.
The results of the infusions were astonishing. Screenings showed Davis’ tumor, which had originally measured more than 2.5 inches, had been completely eradicated. Although she and Dr. Costin don’t know if she received immunotherapy or the placebo, the malignancy “literally melted away, which would be very unusual if you were getting chemotherapy alone,” he says. “We suspect that she got pembrolizumab, but either way, she had a terrific response. And this is why clinical studies are so important, because they’re entering into the frontier.”
Sweet Victory
In May 2020, Davis had surgery to remove the last, tiny traces of her cancer. She was nervous, but Dr. Weiser had long ago won her confidence. “I told him I was going to put my trust in him, and I wanted him to understand that I’d already asked God to guide his hands,” she says.
Using minimally invasive techniques, Dr. Weiser took out the lingering remnants of the malignancy, an area which measured only a couple of milli¬meters. “There was no residual tumor in something that had once been the size of a golf ball,” Dr. Weiser notes. He removed several lymph nodes for testing, as well, and they were cancer-free. “Renee did great with the surgery,” he says, adding that she returned home after just three days.
Dr. Costin gave Davis maintenance medication to further minimize the risk of a recurrence. She finished the regimen in March of 2021. “I would tell anyone in my situation to go to White Plains Hospital,” Davis says. “I thank God every day that I’m alive.”
She was especially grateful that she was able to attend her son’s wedding. “I thought, I made it!” she shares. It was a cherished chance to see her son begin a new, happy chapter of his life — while she began a new, healthy chapter of her own.
To learn more about White Plains Hospital’s Center for Cancer Care, visit wphospital.org/cancer.
Bring Plastic to the Girl Scout House
- Details
- Written by: Joanne Wallenstein
- Category: Health
 (Here's a letter from Girl Scount Troop #2688 asking for your help)
(Here's a letter from Girl Scount Troop #2688 asking for your help)
Dear Scarsdale Residents and families,
We are Girl Scout Troop #2688 and we have a mission. We need to collect 500 lbs. of clean stretchy plastic that can’t be recycled by the town by the end of the school year.
Some examples of this are: bubble wrap, dry cleaning bags, ziplocs, plastic bags, bread bags, cereal inserts and Saran Wrap from your vegetables.
Why not,simply throw it all out you may ask? Well, we are helping our community and environment by collecting this plastic to make an impact. NexTrex, is a company running a program which will send us a bench made from recycled plastic if we reach our goal. The bench will be placed outside the Girl Scout House for public use.
This kind of plastic is most commonly dumped into landfills and oceans affecting not just life on Earth but also Earth itself. We need your help to reach our goal.
Please join our efforts and drop your plastics at one of our 4 public bins around town: at the Girl Scout House, 37 Wayside Lane around the back/facing the field under the awning. Or we have bins on the porches of 12 Barry Road.; 168 Nelson Road. and 164 Gaylor Road.
See the attached flyer of what we can accept.
-Thank you for your help
7th grade Cadette Troop #2688
What Women Should Know About Their Heart Health
- Details
- Written by: Joanne Wallenstein
- Category: Health
 Contributed by Dr. Shalini Bobra, Cardiology at White Plains Hospital
Contributed by Dr. Shalini Bobra, Cardiology at White Plains Hospital
Heart disease remains the leading cause of death for women in the U.S., accounting for about 1 in every 3 female deaths when combined with stroke, according to the Centers for Disease Control and Prevention (CDC). The organization goes on to say that it is the #1 killer of both African American and White women in this country, while it is either tied with, or second to, cancer for female fatalities in other ethnicities.
These are alarming statistics, made even more so when one considers the CDC’s noting that only 56% of women recognize that heart disease is their leading cause of death.
We should all take a moment to consider what can help women avoid contracting this terrible disease.
Although traditional gender roles no longer hold true in many households, I still see a general disparity in the patients I see. A lot of women bring their husbands in when they show signs of heart trouble; when I ask them how they themselves are doing, the women usually respond, “Oh, I’m fine.” That may well be the case, but putting off regular examinations in favor of other family members’ is never a good idea.
Many women still put themselves last when it comes to taking care of health, putting children, spouses, and their own parents ahead of themselves; as a result, they don’t come in as frequently as they should for checkups. Basic blood tests for the likes of cholesterol and diabetes can catch developing conditions early, and an annual visit with your primary care physician is a must.
One thing that many people dismiss is the simple fact that, unfortunately, COVID-19 is still with us. I see a lot of patients with long COVID who are experiencing chest pain and heart palpitations two or more years since their initial infection. The full impact of COVID-19 on the heart is still being studied, but we know it can cause severe inflammation, raising your risk of blood clots. The bivalent booster is safe and effective, and I strongly advise my patients to stay up to date with their vaccines.
In addition, the pandemic created a mess in people’s schedules, some of which have yet to be corrected. Regular exercise fell by the wayside, accompanied by an increase in unhealthy eating and drug and alcohol use, among other factors.
In fact, the #1 heart health mistake people make remains smoking tobacco, as well as marijuana, now that it has been legalized in so many states, including New York. While the potential effects on the heart of smoking marijuana are still being determined, some studies have suggested that the activity can increase one’s risk of heart disease and heart attack.
Good nutrition, not surprisingly, can play an important role in the fight against heart disease as well. A plant-based diet (like many physicians, (I recommend the Mediterranean diet) can lower the risk of heart disease and stroke by as much as 25% – the same effect that cholesterol medicine can have.  A family history of heart disease is also an indicator that you yourself may develop (or already have) the condition. If you have such a family history, be sure to discuss it with your primary care physician and/or cardiologist.
A family history of heart disease is also an indicator that you yourself may develop (or already have) the condition. If you have such a family history, be sure to discuss it with your primary care physician and/or cardiologist.
Indeed, such healthcare providers can go into more depth with you about ways to avoid developing heart disease, as well as how to properly treat it. Bringing the number of cases and fatalities down – in women, and in all of us – should be a goal for everyone.
Dr. Shalini Bobra is a cardiologist with White Plains Hospital Physician Associates, seeing patients at 99 Business Park Drive in Armonk. To make an appointment, call 914-849-7900.