White Plains Hospital’s Team-Based Approach to Multiple Sclerosis Care
- Details
- Written by: Joanne Wallenstein
- Category: Health
 The following interview with Dr. Ute Traugott and Dr. Samantha Epstein, Neurology was submitted by White Plains Hospital.
The following interview with Dr. Ute Traugott and Dr. Samantha Epstein, Neurology was submitted by White Plains Hospital.
Cases of multiple sclerosis (MS), a chronic progressive autoimmune disease that affects the central nervous system, are on the rise in the United States, impacting nearly 1 million people nationwide – with the number of cases nearly quadrupling between 1994 and 2017, according to the National Multiple Sclerosis Society (NMSS).
Improved diagnostic techniques and increased public awareness have contributed to the rise in diagnoses. Risk factors for the condition can include having a first-degree relative with MS or another autoimmune disease as well as vitamin D deficiency and lifestyle factors such as diet, stress, and obesity.
White Plains Hospital is the only healthcare organization in Westchester to have a Multiple Sclerosis Center designated as a Partner in MS Care Center for Comprehensive MS Care by the National Multiple Sclerosis Society. This MS Center offers a variety of services for the diagnosis, treatment and support necessary for living a fulfilling life with MS. Two of its neurologists, Dr. Ute Traugott, Director of White Plains Hospital’s Multiple Sclerosis Center, and Dr. Samantha Epstein, recently sat down to provide information about the Hospital’s approach to the disease.

What are some of the common symptoms of MS, and how is it diagnosed?
Dr. Epstein: In patients with MS, the immune system attacks and damages the central nervous system – the brain, spinal cord, and optic nerves. That damage can result in a variety of symptoms, most notably weakness, numbness and tingling, vision problems, fatigue and difficulties with coordination and balance.
Every MS patient’s journey is different, since symptoms and the disease can vary greatly and are unpredictable, making it a complex condition to manage. There is no single diagnostic test; instead, MS is diagnosed through a combination of clinical history, neurologic examination, ophthalmologic examination, imaging (MRI), blood tests and, if necessary, evaluation of spinal fluid.
What are some of the latest advancements in treating the disease?
Dr. Traugott: All currently available FDA-approved disease modifying therapies (DMTs) for MS are focused on interfering with the migration of activated immune cells from the blood into the central nervous system. This can be achieved by reducing the number of white blood cells through the use of medications that prevent them from multiplying, trapping them in lymph nodes, or by destroying some with the help of monoclonal antibodies. These treatments slow down the progression of the disease and decrease disability.
New therapies that reduce the more widespread inflammation within the central nervous system are expected to become available in the coming year. Several additional medications are currently in clinical trials, one of them focusing on repairing the damage to the myelin, the sheath that forms around the nerves, caused by the disease.
What should a patient look for in an MS center?
Dr. Epstein: Look for neurologists with expertise in diseases affecting the central nervous system who are experienced navigating the complexities of the disease and the ever-growing array of therapies. Additionally, it is important to have access to diagnostic techniques like high-resolution MRI, an infusion center, and the support staff required to help patients through their MS journey.
Dr. Traugott: Certification by the National Multiple Sclerosis Society is very important, as it assures patients that there is a highly-qualified group of specialists forming a treatment team to provide the necessary comprehensive care. The team usually includes rehabilitation specialists, occupational and speech therapists, urologists, radiologists, neuropsychologists, psychiatrists, neurophysiologists and more.
What are some of the other benefits MS patients can access at White Plains Hospital? 
Dr. Traugott: I have more than 30 years of experience in treating MS patients. I am a founding member of the Neuroimmunological Society and have received awards for my contributions to the MS field by the National Multiple Sclerosis Society and by the American Academy of Neurology. Dr. Epstein, who recently joined us, also has a lot of experience in the care of those patients. Our MS-certified RN, Taylor Maloney, provides valuable advice to our patients and can answer many questions they may have. Tammy Schoenfarber, our social worker, is available for counseling newly-diagnosed patients as well as for those who face some challenges later on.
We work closely with Burke Rehabilitation Center and White Plains Hospital’s outpatient physical therapy practices for many of our patients’ rehab needs. We can also refer patients to physicians or other specialists at the Hospital, and to our infusion center.
Learn more about Multiple Sclerosis Services
Dr. Ute Traugott is a specialist in Neurology, Multiple Sclerosis and Neuroimmunology and the Director of White Plains Hospital’s Multiple Sclerosis Center. To make an appointment, call 914-681-1126.
Dr. Samantha Epstein is a board-certified neurologist whose specialties include Multiple Sclerosis and Neuroimmunology. Dr. Epstein sees patients at White Plains Hospital Medical & Wellness in Armonk and WPHPA in Harrison. To make an appointment, call 914-849-5300.
Health Matters
The original version of this article was published in Health Matters, a White Plains Hospital publication.
Key Campaign Highlights 7 Reasons Why Underage Drinking is a Big Deal
- Details
- Written by: Wendy MacMillan
- Category: Health
 Anyone who has had the pleasure of spending time at Scarsdale High School knows what thoughtful, dedicated, and hardworking teenagers we have here in the ‘Dale. It surprises no one when we hear about our teens being recognized for their volunteerism, for their science research projects, for their athletic prowess, or for their incredible artistic abilities. Perhaps, however, it would surprise some in our community to learn that Scarsdale teens’ alcohol consumption is significantly higher than the national average.
Anyone who has had the pleasure of spending time at Scarsdale High School knows what thoughtful, dedicated, and hardworking teenagers we have here in the ‘Dale. It surprises no one when we hear about our teens being recognized for their volunteerism, for their science research projects, for their athletic prowess, or for their incredible artistic abilities. Perhaps, however, it would surprise some in our community to learn that Scarsdale teens’ alcohol consumption is significantly higher than the national average.
In fact, according to Scarsdale Action for Youth (SAY), data from the annual PRIDE Survey reveals that in 2024, 20% of Scarsdale Middle School 8th graders (12 year olds) reported alcohol use, compared to 12% nationally; and 67% of SHS 12th graders reported alcohol use, compared to 41% nationally. The survey also makes clear that here in Scarsdale, the largest jump in teen alcohol consumption is seen in 9th and 10th grades with big increases in use occurring in the springtime around events like graduation and prom.
There are likely a variety of factors that contribute to underage drinking amongst Scarsdale teens: easy access to alcohol in the home, parents who are more complacent, older siblings who might buy alcohol for their younger siblings just to name a few…but whatever the reasons, given the harmful effects alcohol can have on a developing brain and the fact that early alcohol use increases risky behavior, poor grades, and future addiction, SAY encourages parents to do more to discourage their kids from underage drinking.
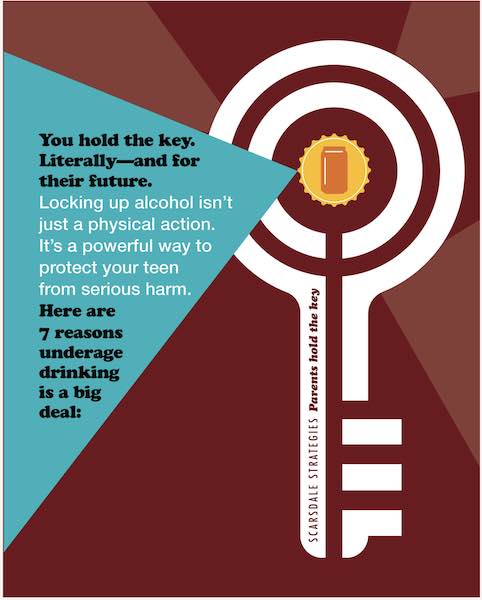
In their new “KEY” campaign, SAY outlines the pitfalls of early alcohol use and reminds parents that “Teens face pressure, curiosity, and opportunity, often right at home. Talk with them about alcohol and how it hurts their wellbeing. Set clear expectations. And to reduce risk, monitor what’s in your home and lock your liquor. Locking up alcohol isn’t just a physical action. It’s a powerful way to protect your teen from serious harm.”
The annual PRIDE survey further reveals that 40% of middle school students reported that parents either never or seldom discussed problems with drug and alcohol use with them. Another 37% reported that parents discussed the repercussions of alcohol use “only sometimes.” The Key Campaign highlights these 7 reasons why underage drinking is a big deal and encourages parents to talk about these issues with their young teenagers.
It interferes with brain development, especially in areas tied to decision-making and impulse control.
It can increase the risk of mental health issues like anxiety, depression, and suicidal thoughts.
It can lead to risky behavior, including impaired driving, unsafe sex, and violence.
It can damage academic performance, causing poor grades, missed classes, and lower achievement.
It raises the chance of addiction later in life, especially when drinking starts before
age 15.
It affects sleep and mood regulation, which are already fragile during teen years.
It can result in legal trouble that impacts college, jobs, and their future opportunities. Getting caught with a fake ID is a felony and can result in up to a 7-year jail sentence.
Unfortunately, the list doesn’t end here. Learn more here.
Research also shows that parents are the #1 reason why teens refrain from drinking, so parents truly hold the key to whether or not their teenagers drink. In addition to having important discussions with their teens, the Key campaign encourages parents to be proactive about helping teens avoid temptation. With Scarsdale teens admitting that it is easy for them to get their hands on alcohol (namely from a parents’ home bar) and that they are most likely to drink at home or at a friend’s house, SAY recommends the following actions to take:
-Lock up your liquor. SAY suggests these handy locks for cabinets and fridges:
-Count your beers. Keep inventory of your beers and alcoholic beverages.
-Dye clear liquor to prevent it from being watered down.
-Supervise the basement parties at your house and be clear about rules in your house. Remember that Westchester has a social hosting law, which means you are liable if alcohol is served to minors at your house.
For more tips and strategies or to learn more about the Key Campaign check out Scarsdale Action for Youth website here and follow SAY on Facebook, Instagram, or X.com.
White Plains Hospital to Enhance Emergency Care
- Details
- Written by: Joanne Wallenstein
- Category: Health
 In 2024, White Plains Hospital’s announced its largest expansion project to date: a 10-story, 475,000-sq.-ft. state-of-the-art facility opening in early 2028. While this new expansion will address the growing demand for high-quality care in our community, one significant feature will be the new Emergency Department that will more than double the size of the Hospital’s current ED.
In 2024, White Plains Hospital’s announced its largest expansion project to date: a 10-story, 475,000-sq.-ft. state-of-the-art facility opening in early 2028. While this new expansion will address the growing demand for high-quality care in our community, one significant feature will be the new Emergency Department that will more than double the size of the Hospital’s current ED.
“For many of our patients, the Emergency Department is the first touchpoint with our Hospital,” says Dr. Dean Straff, Director of Emergency Medicine. “In fact, 80% of patients who are admitted to the Hospital first begin their journey in the ED.”
White Plains Hospital’s Emergency Department continues to be the busiest in Westchester County. Patient visits have grown more than 66% since 2010, with nearly 90,000 visits projected in 2025, and more than 20% of these patients requiring hospitalization.
The new, expanded Emergency Department will connect to the existing care space and feature:
-An additional 22,650 sq. ft. of space
-More than 100 state-of-the-art care spaces, nearly double the current capacity
-A dedicated driveway for drop-off and entering the ED
-Expanded ambulance bays
“This new expansion will ensure that we can continue to provide the highest quality of care in an efficient manner to all those who come through our doors,” says Dr Straff.
“Over the years, the Hospital has continued to build out its capabilities, adding new, advanced services to support our life-saving work. This new expansion is critical to our growth, ensuring we will always be able to meet the immediate needs of our community,” he continues. “Patients trust us to provide the best care during critical moments. Whether it is a child with an ear infection, or an individual requiring life-saving attention for a stroke or cardiac arrest, our talented team is always prepared to provide the award-winning care that distinguishes White Plains Hospital as a leader in safety and quality.”
Stay up to date on this exciting expansion and learn how to support our efforts to transform the future of care in the Hudson Valley.
Health Matters
The original version of this article was published in Health Matters, a White Plains Hospital publication.
Advanced Care for Kids, Close to Home
- Details
- Written by: Joanne Wallenstein
- Category: Health
 (This article was submitted by White Plains Hospital)
(This article was submitted by White Plains Hospital)
Living in Westchester County brings many benefits, including good schools, recreational spaces, cultural offerings, and more. Improved access to pediatric subspecialty care is yet another advantage for Westchester families. The recent expansion of the White Plains Hospital Pediatric Specialty Center—a partnership between White Plains Hospital and the renowned Children’s Hospital at Montefiore Einstein (CHAM)—has brought to the region convenient pediatric subspecialty care that parents elsewhere have to travel far and wide to access.
“With only approximately 400 pediatric rheumatologists in the U.S., very few families have access to a pediatric rheumatologist right in their community,” says Dr. Michael Cabana, Physician-in-Chief at CHAM and Chair of Pediatrics at Albert Einstein College of Medicine. That won’t be an issue here in Westchester.
“We are pleased to bring even more renowned pediatric subspecialists to care for our youngest patients close to home at White Plains Hospital,” adds Frances Bordoni, Executive Vice President for Ambulatory and Physician Services and Business Development at White Plains Hospital. “Removing the need to travel to receive high-quality care for their children saves time and peace of mind for busy parents in the Hudson Valley, allowing them to focus on what matters most.”
With the expansion, seven additional providers are available at the White Plains Hospital Pediatric Specialty Center, which is now home to 23 pediatric subspecialists from Montefiore. The physicians see patients at the Center’s offices at 33 Davis Avenue in White Plains, at Scarsdale Medical Group in Harrison and at the Hospital’s Center for Advanced Medicine & Surgery.
They specialize in a range of pediatric care including:
• Adolescent medicine
• Pediatric cardiology
• Endocrinology (including juvenile diabetes and bone health/growth care)
• Gastroenterology
• Nephrology
• Orthopedics
• Otolaryngology
• Pulmonology
• Rheumatology
• Surgery
Highly trained physicians of this kind are in short supply nationwide. “It’s ironic—we have better therapies than ever for kids who need specialty care, yet many people don’t have access to a subspecialist,” explains Dr. Cabana. “That’s why this Center is really important.” Pediatric GI specialists, for instance, are experts in treating irritable bowel diseases like Crohn’s disease and ulcerative colitis. Urologists can address conditions such as prenatal hydronephrosis, or the swelling of a kidney in a fetus or infant. Pulmonologists offer long-term care for children with asthma.
“We’ve got everything covered,” Dr. Cabana says. “There are so many things we can do in pediatric care now that we couldn’t do when I trained as a pediatrician 30 years ago. Our job is making sure those therapies are accessible and that kids get the very best care, at the right time, as conveniently as possible.”
In fact, the outpatient treatments provided at the Pediatric Specialty Center are so successful, they are able to prevent most pediatric patients from needing hospital admission. “We can use great new medicines like monoclonal antibodies, which have been available to adults for the past two decades, to help prevent flare-ups and hospitalizations for kids with chronic diseases,” Dr. Cabana says.
If a child’s condition gets to the point where they require hospitalization, they benefit from the seamless coordination of care between White Plains Hospital and CHAM, which ensures continuity and expertise at every step. This collaborative approach enables patients access to CHAM’s Pediatric Heart Center, a world leader in advanced cardiovascular care for patients with congenital heart diseases, as well as its renowned pediatric surgery services and comprehensive program for children with kidney problems, including New York state’s first dedicated pediatric dialysis facility.
Dr. Cabana notes that the Pediatric Specialty Center is the latest benefit of the partnership between
White Plains Hospital and Montefiore
“Many of our physicians actually live in Westchester, so the local connection is very strong,” he adds. “I am so proud of these providers, and now, with even more physicians we can care for a greater number of patients in Westchester and the lower Hudson Valley.”
To make an appointment at the White Plains Hospital Pediatric Specialty Center, call 914-849-KIDS (5437) or view the list of doctors at the White Plains Hospital Pediatric Specialty Center.
Health Matters
The original version of this article was published in Health Matters, a White Plains Hospital publication.
Over 500 Runners Participate in the 55th Annual 15K & 4 Mile Run
- Details
- Written by: Sharon Higgins
- Category: Health
 On Sunday, April 6th over 500 runners took their marks to participate in Scarsdale’s 55th Annual 15 Kilometer and 4 Mile Road Races. The races were organized by the Village’s Department of Parks, Recreation and Conservation. Superintendent Brian Gray was extremely happy with the turn out and smooth running of the races by his staff and community volunteers as well as the Scarsdale Police Department, Scarsdale Fire Department, Scarsdale Volunteer Ambulance Corp and Scarsdale Department of Public Works, who all worked in various roles to support this event.
On Sunday, April 6th over 500 runners took their marks to participate in Scarsdale’s 55th Annual 15 Kilometer and 4 Mile Road Races. The races were organized by the Village’s Department of Parks, Recreation and Conservation. Superintendent Brian Gray was extremely happy with the turn out and smooth running of the races by his staff and community volunteers as well as the Scarsdale Police Department, Scarsdale Fire Department, Scarsdale Volunteer Ambulance Corp and Scarsdale Department of Public Works, who all worked in various roles to support this event.
Mr. Gray commented: “as I left my house it was pouring rain and I was questioning whether or not runners would turn  up. Thankfully, as I arrived in Scarsdale and was doing my pre-course drive-through, the rain slowed and temps rose to optimal conditions for running. After reflecting on Sunday’s event, I look back on the 18 years I have been the Race Director of the Annual Road Races. One of the most satisfying things to witness is the community support of residents cheering runners on with handmade signs and banners, and in a few cases, setting up water stops for runners along the course.”
up. Thankfully, as I arrived in Scarsdale and was doing my pre-course drive-through, the rain slowed and temps rose to optimal conditions for running. After reflecting on Sunday’s event, I look back on the 18 years I have been the Race Director of the Annual Road Races. One of the most satisfying things to witness is the community support of residents cheering runners on with handmade signs and banners, and in a few cases, setting up water stops for runners along the course.”
The weather outside was a cool 45 degrees and overcast. The air was a bit damp but besides that the conditions for the races were ideal. This year, there were a total of 597 registrations with 521 (87%) showing. This is up slightly from last year with 588 registrations and 487 (83%) showing. There was a healthy spread of veterans and newcomers. I spoke with participants as they got ready for the race, collected their numbers, and grabbed water or a snack. Many indicated that they have been participating in this particular race for years while others said it was their first road race ever. Some were serious runners and others were simply there for a “fun run” and admitted to walking hills if that is what it took to finish.
At a little before 9:15am, at the corner of Harcourt and Hampton Roads, the 4 Mile registered runners of all ages— including parents pushing their children in jogger strollers— lined up to start the race. Instructions and well wishes were given to the runners over a microphone by a Scarsdale Park, Recreation and  Conservation representative. The air horn sounded and they were off.
Conservation representative. The air horn sounded and they were off.
At this time, the 15K runners were making their way to their race starting line, just feet away from the entrance to the high school on Brewster Road. Announcements on the course layout supported by lawn signs and finish line were given as well as a quick address from Scarsdale Mayor Justin Arest. Right before the air horn blew at 9:30am, a PRC representative gave a final call to be careful of possible wet patches even though the streets had been cleaned by the town and therefore they should “run their personal best; it is perfect weather for it!”.
Runners in both races ran loops marked with lawn signs indicating race directions in the Fox Meadow and Greenacres neighborhoods with hills and flats scattered throughout the courses. Police blocked the race roads from traffic to ensure the safety of the participants and a police motorcycle escorted the last runners. Water tables were set up along the course manned by volunteers and PRC representatives.
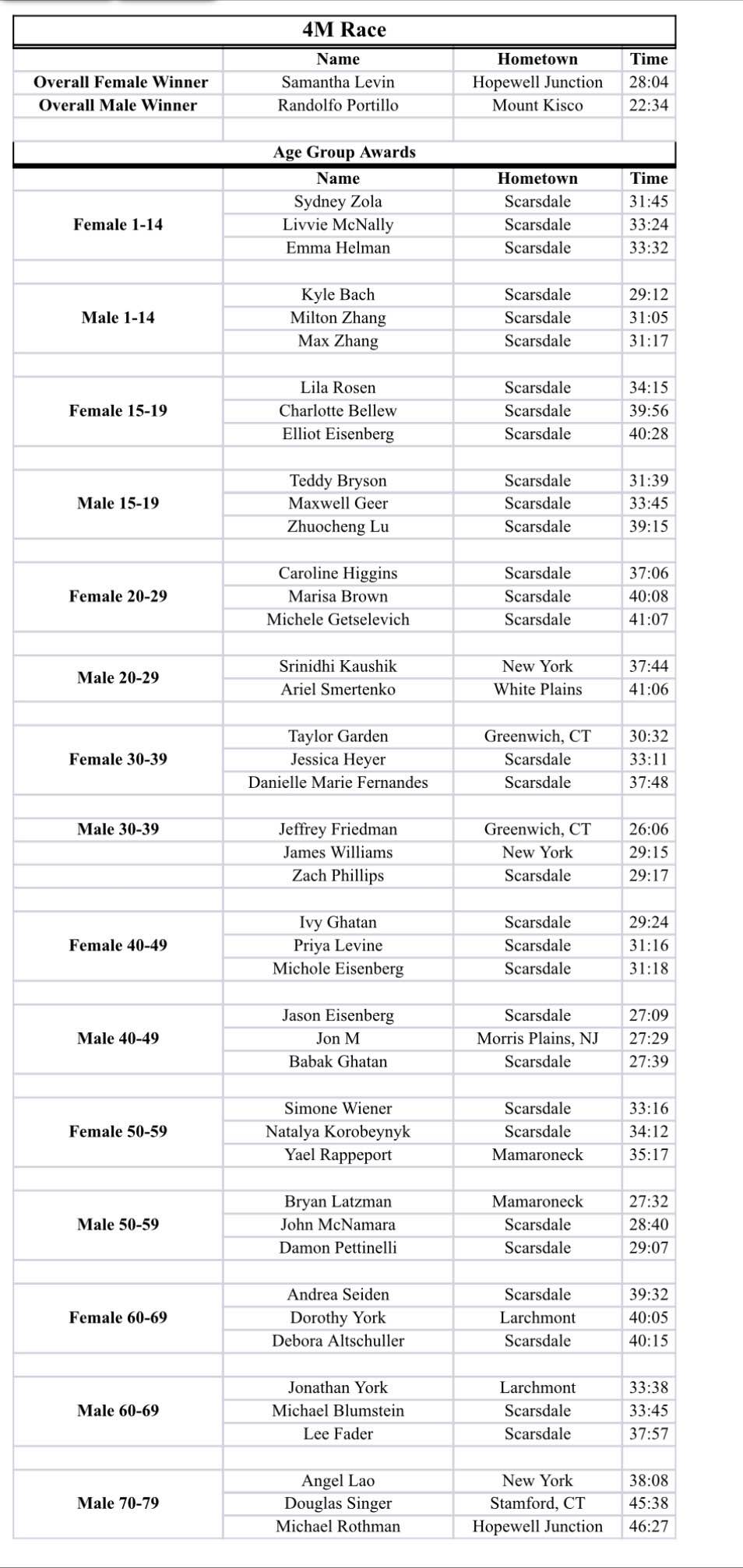
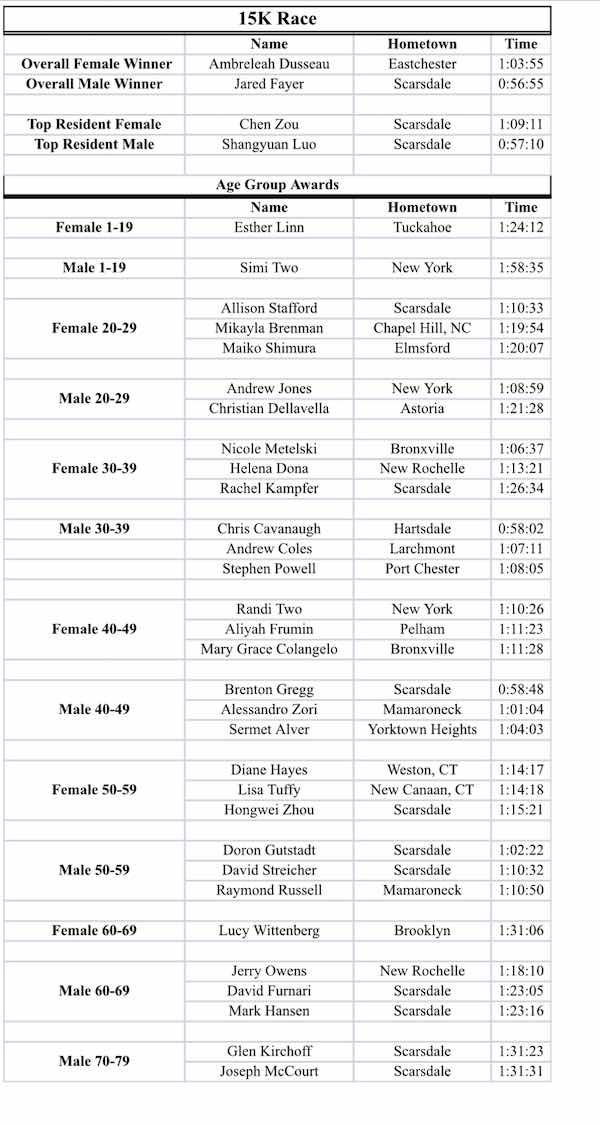
 In twenty two minutes thirty four seconds, with spectators cheering him on, Randolfo Portillo of Mount Kisco was the first runner of the 4 Mile Race to cross the finish line set up a little more than halfway around the Scarsdale High School track. Cheers continued from friends and family members as participants ran across the finish line for the next 55 minutes. Runners made their way into the high school circle. The Scarsdale Fire Department had set up a ladder truck bearing a gigantic American flag. Participants ran under the flag on their way to the last stretch of the course around 2/3 of the track with the finish line set up by the bleachers. With most of the 4 Mile runners through, the crowd roared for Jared Fayer, a Scarsdale resident, who finished first in the 15K race with an impressive time of 56 minutes and 55 seconds.
In twenty two minutes thirty four seconds, with spectators cheering him on, Randolfo Portillo of Mount Kisco was the first runner of the 4 Mile Race to cross the finish line set up a little more than halfway around the Scarsdale High School track. Cheers continued from friends and family members as participants ran across the finish line for the next 55 minutes. Runners made their way into the high school circle. The Scarsdale Fire Department had set up a ladder truck bearing a gigantic American flag. Participants ran under the flag on their way to the last stretch of the course around 2/3 of the track with the finish line set up by the bleachers. With most of the 4 Mile runners through, the crowd roared for Jared Fayer, a Scarsdale resident, who finished first in the 15K race with an impressive time of 56 minutes and 55 seconds.
Names and times of all winners in each category for each race are listed in the tables below. Congratulations to all the participants and workers of the event. You are all winners!